What is Bladder Health? Is this bladder irritation IC/BPS?!
Many things can contribute to your overall bladder health -How much water you drink, what you consume, how you use the bathroom, and if you are pushing down and pressuring the bladder all affect the function and health of your bladder and urinary functions! I know--So much more than we were ever taught!
Many people that experience bladder discomfort, frequent irritation, or discomfort with urination take to Google and Reddit, ending up panicked over the possibility of IC/BPS. Don’t fret- we have helped many people walk this journey- and can often eliminate symptoms before needing to go for testing. American Urological Association gives the highest efficacy rating to pelvic floor therapy in dealing with symptoms, above most medications or procedures.
What is Interstitial Cystitis (IC) or Bladder pain syndrome (BPS)?
Did you know there is an estimated 5% of people living with IC/BPS – that is 1 in 20 people!
The American Urological Association (AUA) defines IC/BPS as “an unpleasant sensation (pain, pressure, or discomfort) perceived to be related to the urinary bladder, associated with the lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes” (Clemens, 2022).
Who does it effect and how is it diagnosed?
Our understanding of IC/BPS has evolved in the recent years. While we used to think this condition was primarily only present in women, it is also prevalent in men. IC/BPS occurs throughout the lifespan. Historically diagnosis for IC was following cystoscopy confirming Hunner’s lesions in the bladder.
However, you can have valid symptoms and diagnosis of IC/BPS without having these lesions on the bladder. In fact, your bladder can look completely “fine” on a cystoscopy and you could still have IC/BPS.
More often than not the bladder is not the sole culprit, there are many factors at play-the nerves, the pelvic floor, what we eat and drink, stress management and day to day activities that could be contributing to the increase or decrease of symptoms. No 2 IC/BPS symptoms or cases are identical- it takes a tailored approach to address the root cause, not a single diet or medication like we one believed.
Pelvic Floor Therapy
Manual pelvic therapy techniques are given an evidence Grade “A” by the AUA. With pelvic floor dysfunction being common for clients with IC/BPS (and often a driver of pain), pelvic floor therapy helps to decrease symptoms and break the pain cycle.
Bloom Pelvic Therapy specializes in treating IC/BPS, finding the root cause (or most often causes) of dysfunction, working along side your medical team to help you decrease & manage the symptoms. An evaluation looks your whole body- toes to crown of your head, movement, what a typical day looks like, what is going in the body (via food, drinks, medications, vitamins), how the bladder and bowels are functioning (yes the bowels- they are a huge contributor to bladder health and function), and what you have attempted this far in your journey. From there the pelvic floor therapist will help to put together the pieces and explain the plan to help you reach your goals.
Depending on what is found in the evaluation the pelvic therapist tailors treatment approach- often this includes movement- either in the form of gentle exercise, modifications for form, stretching, or strengthening. We promise we will never forbit or restrict your beloved movement or exercises- we may work together to modify, but we are big believers in keeping the things we love for optimal quality of life.
Never do we include Kegels as part of the treatment- this often makes symptoms much worse, especially for those experiencing IC/BPS symptoms. Each visit, clients leave with actionable items to complete between visits.
IC Diet- Whats up with this?
There is no “IC Diet” that works for everyone. You will find these to be extremely extensive and restrictive. While there may be a few foods that could trigger symptoms for certain folks (i.e., caffeine/coffee, wine/alcohol, citrus like lemons and limes, tomatoes/sauce, and spicy food), this does not impact everyone’s symptoms.
In fact, these things can also irritate people who don't have IC/BPS! Instead of refraining from eating or drinking certain things, it can be helpful to have awareness to see if these things contribute to any pain or urgency/frequency flares.
Medications
Certain medications like Elmiron may not be the answer to all of your IC/BPS symptoms, especially if your bladder lining is not the issue.
There also can be serious side effects to consider with your prescribing physician – take a peek at the warning label on this. You should not delay essential treatment, such as pelvic floor therapy, as you are waiting to see if this medication will work for you.
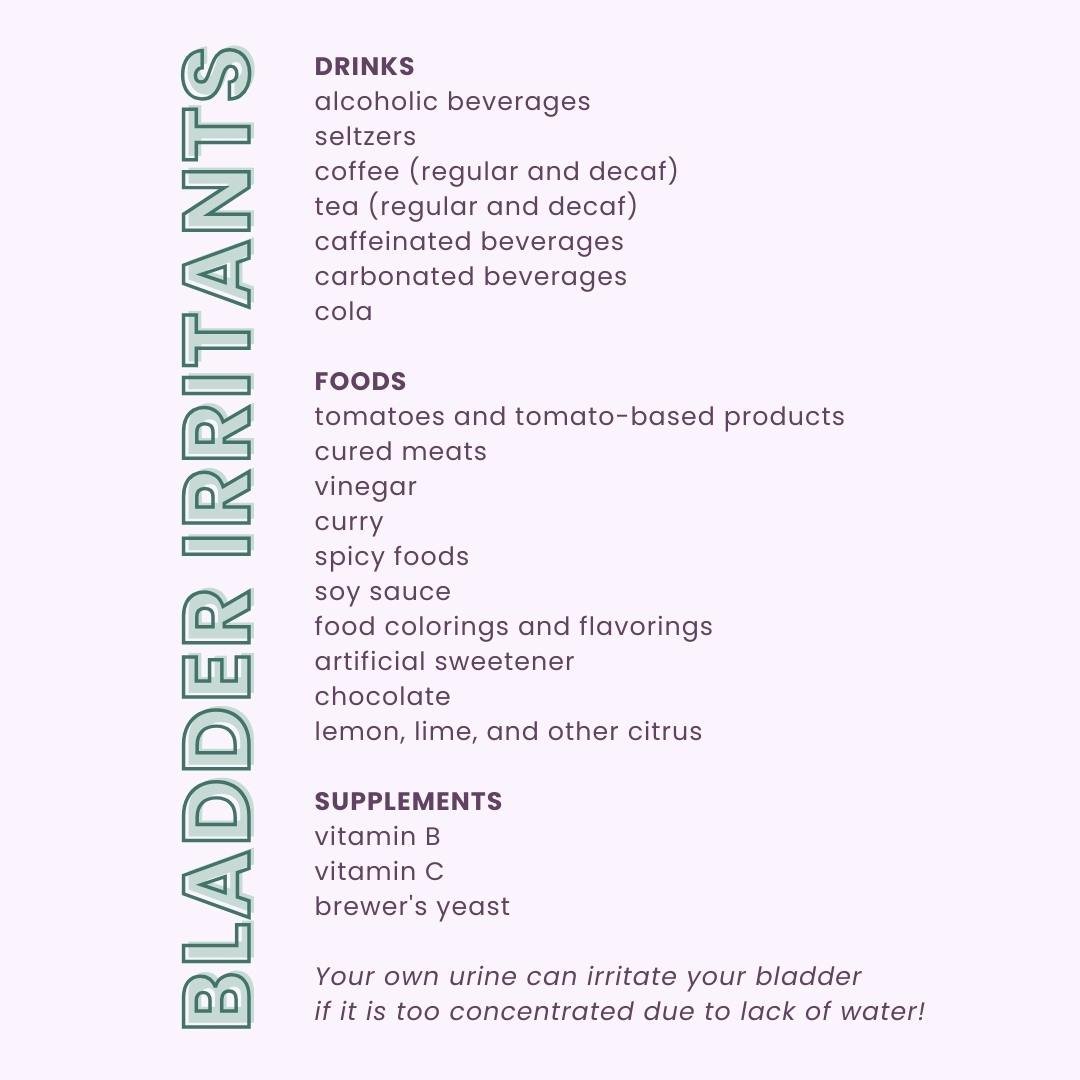
Looking for a list of bladder irritants?!
Remember, you do not need to give these items up completely!
If you are choosing to consume coffee or any of the other irritants listed, we recommend matching the amount in water.
For example, if you consume 12oz of a liquid irritant, drink 12 additional oz of water. Being mindful is key and learning more about how unique your body is will help you in the long run!
If you are experiencing symptoms, know that you are not alone!
We are here for you and understand the importance of being heard and treated with a custom treatment plan-
it's not just "in your head!"
Call us (813) 515-9008 to book an appointment with a pelvic floor therapist at Bloom!