It Feels Like Something is Falling Out: Will Pelvic Floor Therapy Help Me?
So often we hear our clients concerned about feeling or seeing a bulge down there, at times clients report the sensation of something “falling out”. Yes- pelvic therapy helps prolapse! Yes- you can avoid surgery for most cases of prolapse! Our pelvic floor physical and occupational therapists are well-versed in Pelvic Organ Prolapse or POP, and can help!
What is prolapse?
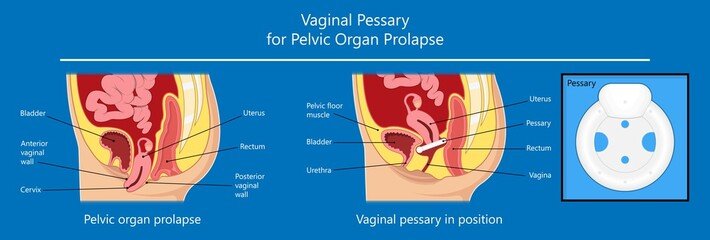
Pelvic Organ Prolapse (POP), commonly referred to as simply “prolapse,” is when one of the neighboring organs in the pelvis, such as the bladder, uterus, or rectum, pushes into the vagina or onto the vaginal walls.
We commonly hear the following from our clients experiencing prolapse:
“It feels like something is falling out.”
“My vagina feels heavy.”
“It’s like a constant pressure that gets worse after being very active.”
“I feel a bulge when I’m washing myself.”
“I can feel something against my underwear that wasn’t there before.”
“I’m scared to do anything. I’m afraid to make it worse.”
How do I know if I have a prolapse?
Prolapse is assessed using a system either called the Baden Walker System or the POP-Q, which provides a grade or stage for organ descent between 0 and 4. This is a fancy way of saying that there is a classification system used to notate the severity of prolapse anatomically. This can be done with the naked eye, palpation, and sometimes with measuring tools. Some physicians may choose to have you complete further diagnostics, such as an ultrasound, to determine the degree or grade of prolapse.
If you suspect you may have prolapse, you may find a qualified pelvic floor therapist near you for an evaluation and treatment to start reducing prolapse symptoms right away. Some people may choose to bring this up to their gynecologist. If your prolapse is considered a grade or stage 1 or less, many medical professionals do not consider this a “true prolapse.” However, just because the severity may be minimal does not mean that your symptoms are not real. If your doctor finds that you do have pelvic organ prolapse, they may refer you to a pelvic floor therapist or they may recommend a urogynecologist for surgery.
Most people are surprised to find out that many women have some sort of minimal prolapse, yet are completely unaware. Others may have a prolapse, whether considered minimal or more severe, and are highly aware, with symptoms interfering with their quality of life and day to day activities.
When you are assessed for pelvic organ prolapse, it is important to be evaluated at some point in a standing position. The impact of gravity and being in an upright position can be quite significant when it comes to prolapse. This is why your symptoms may feel different when you are standing vs. lying down at times. Your pelvic floor therapist will assess your pelvic floor and any laxity of the vaginal walls due to organ descent as they may ask you to activate the pelvic floor muscles, try to release or relax them, and then try to bear down to approximate what occurs when there is a rise of intra-abdominal pressure.
Why do I have prolapse?
There are many risk factors for prolapse. Many clients are relieved to hear that it was not one specific workout they did or one wrong move they made that “caused” their prolapse. It can be helpful to note that a number of factors may have contributed to their prolapse symptoms and even predisposed them to be at a greater risk for developing prolapse.
Common risk factors include:
Family history of prolapse
History of constipation
Frequent straining from constipation or activities
Chronic cough
Asthma
BMI greater than 25
Repetitive, heavy work
Vaginal birth
Vaginal birth with forceps assist
Levator ani avulsion (injury to pelvic floor muscles)
Connective tissue disorders or concerns
How will pelvic floor therapy help my prolapse?
When working with a pelvic floor therapist, your plan may include some or all of the following:
Education to help you better understand your symptoms
Strengthening pelvic floor muscles with whole-body exercises
Hands-on manual techniques to decrease pelvic floor or surrounding muscle tension
Daily posture modifications
Lifestyle and habit modifications
Pressure management and decreasing strain on your pelvic floor from coughing, constipation, exercise, caregiving, etc.
You may or may not see a change in the “grade” or “stage” of prolapse as you see an improvement in your symptoms. This is completely dependent on the person, the degree of prolapse, and the cause(s) of their prolapse. Pelvic floor therapists are equipped to help you improve your quality of life, get you back to doing the things you love with confidence, and help you get ahead of any issues down the road. We see you, we hear you, and we are happy to be alongside you to help you feel more like yourself again.
How long does it take to fix a prolapse?
We get this question over and over again at our clinic. When it comes to “fixing” any type of pelvic floor dysfunction, we are here to first remind you that you are not broken. You are human!
What you are experiencing is very real and can feel extremely isolating or like you are completely alone dealing with these issues. We hope it is supportive to hear that it is more common than you may think with how little people discuss these topics. We hope that it is even more encouraging to know that pelvic therapy can help to bring you relief from your prolapse symptoms.
How long it takes to find that relief depends on the person and the severity of not only their degree or stage of prolapse but also their level of symptom-bother. Additional factors also contribute to the recovery timeline including daily physical demands, co-occurring constipation, age and stage of life, and more.
Some clients may find their symptoms have started to ease up even after the first few pelvic therapy appointments and as they started to incorporate some of their home exercise program outside of the clinic. These clients should continue to see continued improvement of symptoms as they progress in their plan of care. It is important to note that progress is not always linear. Depending on the demands of the day, exercise, stage of menstrual cycle, hormones, cold & flu season, etc., it is normal for symptoms as well as symptoms relief to fluctuate while overall trending towards symptom relief.
Will I need surgery for prolapse?
Many of the clients we see come into our clinic with the desire to avoid surgery if it is not needed. We are here to provide a number of effective non-surgical options to provide support and symptom relief while collaborating with your medical care team to ensure the most effective outcomes for you. We have worked with many clients of all ages with prolapse that are happy to have found symptom relief without having to jump to a surgical option right away.
Depending on the type and level of prolapse, your pelvic floor therapist may recommend adding a urogynecologist to your care team for additional evaluation and support. This does not mean that the pelvic floor therapist thinks your concerns cannot be improved by pelvic floor therapy. When this referral happens, it is likely to ensure you are receiving the most comprehensive care possible and that you are fully informed of the range of treatment options available that can work hand in hand with your pelvic floor therapy progress. Your pelvic floor therapist and urogynecologist may work together to determine if a support option, such as a pessary, would be beneficial for you or if additional medical intervention may be recommended based on your specific presentation of prolapse, as well as your goals.
What are pessaries?
Pessaries are often made of medical-grade silicone and are inserted into the vagina to help support the position of pelvic organs, such as the uterus, bladder, urethra, and rectum. There are a variety of pessary types, and they are fitted or sized specifically to your body. If you are fitted for a pessary and it falls out, feels uncomfortable, or otherwise just does not seem like the right fit for you, it is important to discuss this with your medical team so alternative options or sizes can be tried. Pessary fitting is often considered an art and does require some patience to find the just right fit for you. Some people wear their pessary during more demanding daily activities and others find more support by wearing it more often or around the clock, removing it as recommended for cleansing or per wearing-schedule.
We often have clients that ask if using a pessary is a band-aid, cheating, or not addressing the real problem. The answer is quite the opposite. Providing this support to your pelvic organs can be extremely helpful for your connective tissue that otherwise may be more in a disadvantaged or “stretched” position.
It is important to continue pelvic floor therapy once you are fitted for a pessary. When this support is provided, your pelvic floor muscles may be able to more appropriately rehabilitate, get stronger, and/or decrease in muscle tension to become more responsive as they have the necessary space to do so appropriately. Pessaries in conjunction with pelvic floor therapy can be a game changer in improving quality of life for people experiencing prolapse - now and in the long run!
How do I start feeling like myself again?
Pelvic floor therapy is the perfect starting place as you are trying to understand your symptoms, your body, and how to find relief. Check out our blog on Pelvic Floor Therapy Near Me: How to Find A Pelvic Floor Therapist to make sure you are looking for the right things when searching for a pelvic therapy clinic. At Bloom Pelvic Therapy, we see clients in-person in our South Tampa and Lutz clinics. We also work with clients on their paths to wellness across the U.S. and internationally through telehealth. We are excited that you are taking the time to learn more about your pelvic health and look forward to connecting with you!