Why Do I Have Pelvic Pain?
We often get this question when clients are trying to understand the underlying contributors or root causes of their pelvic pain. There is so much more than meets the eye when it comes to pelvic pain. The truth is that a thorough evaluation of your pelvic floor and your unique body mechanics can help to more accurately determine why exactly you may have pelvic pain.
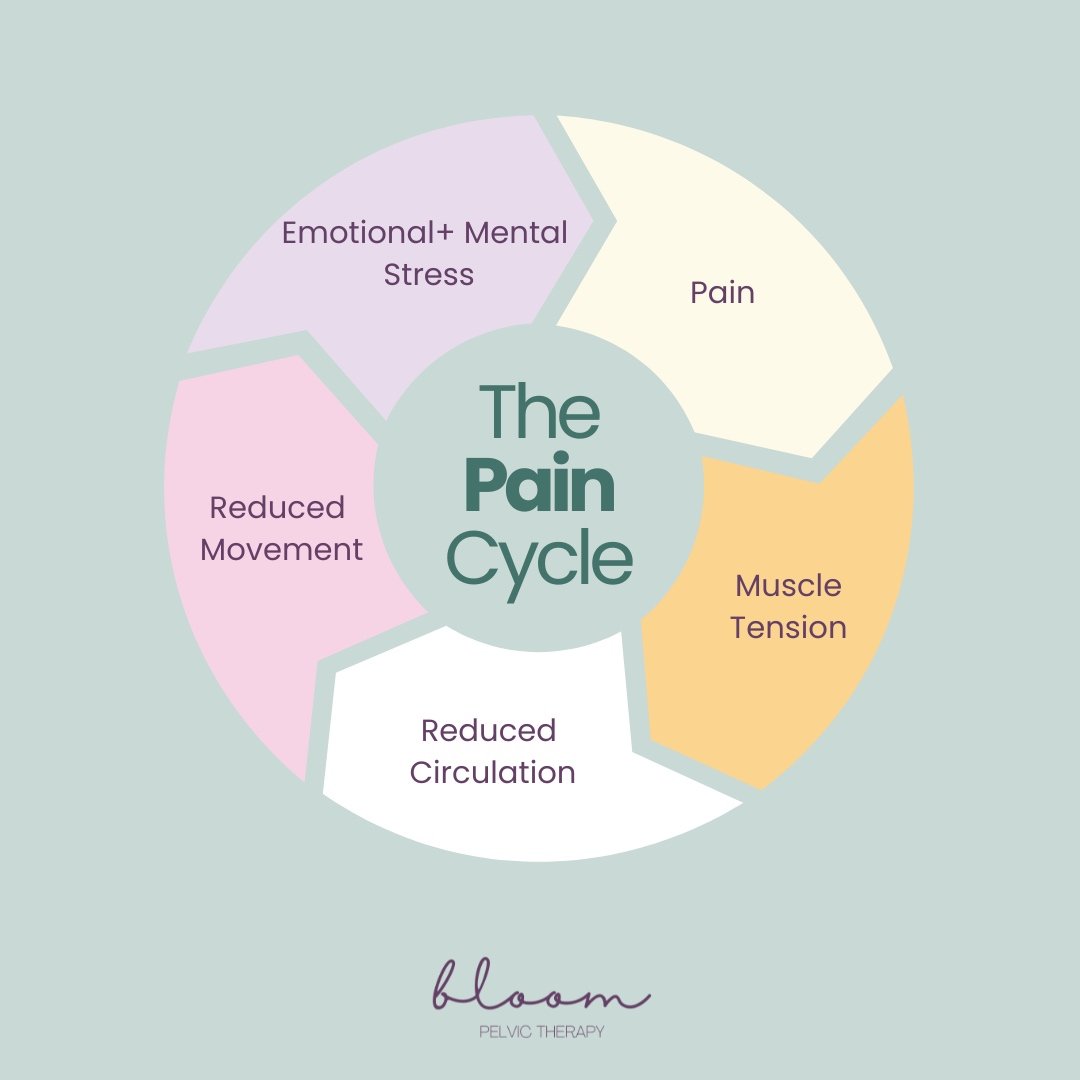
One thing that can be extremely helpful in the path towards healing pelvic pain is gaining an understanding of the pain cycle. This can help to affirm that “No, it is not all in your head!” There is a very real physiological reason for your pelvic pain.
Sometimes what started as a seemingly unrelated incident, such as a fall on your tailbone in childhood, could have set the stage for pelvic floor pain and issues down the line that maybe did not encroach on your daily life until another incident (childbirth, menopause, a hip injury, etc.) brought it to light. It could even be years later when it seems like suddenly all of your pelvic pain began when truly you may be experiencing or noticing the tip of the iceberg when the foundation has been crafted over the past several years. Once you add the pain cycle into that mix, the challenge may seem insurmountable to overcome.
The good news is that you do not have to be alone on your path towards healing. At Bloom, we work with clients experiencing a variety of pelvic pain concerns with varying origins. We are here to support you by first identifying the root cause of your pain and then helping you to address and correct some of the contributing factors so that you can get back to living your best life, pain-free.
Common Causes or Contributing Factors to Pelvic Pain
Listed below are only some of the common causes or contributing factors to the pelvic pain experience. This list is not exhaustive!
Birth injury, vaginal tearing, C-section (no matter how long ago)
Back, abdominal, or pelvic injury or surgery
Orthopedic history
Pudendal neuralgia
Other nerve related dysfunction
Neuroproliferation (increased number of nerve endings)
Past fall on tailbone or vulvar area
Pelvic floor muscle tension or overactivity
Vaginismus (anticipatory pelvic muscle guarding)
Stress, anxiety, nervous system
Hormones
Endometriosis
Pelvic organ prolapse
History of trauma
The 5 Points in the Pain Cycle:
1.First, pain must start. Sometimes, this may be due to an injury. In other cases, it may be due to an underlying condition or a symptom of something else altogether. Pain is produced by your brain and is caused when your brain thinks you are under threat or need protection. However, it is not always immediate. Our brains are constantly evaluating what the most important thing is at any given moment. That is why sometimes pain is not felt instantly, but sometimes days or even weeks later.
To be clear, this does not insinuate that pain is all in your head. In fact, it means the opposite. Your pain is real, it is physical, and it can be decreased or eliminated as you break the pain cycle with pelvic floor therapy.
2. After pain is felt, muscle tension starts. Muscle tension is often associated when feeling pain because the body is reacting to try and protect itself! Sometimes, this is also called muscle guarding.
3. After muscle tension starts, there is reduced circulation to the area and over time leads to muscle inflammation.
4. When areas of the body are feeling tense and inflamed, your brain will compensate and try to avoid using that area, which leads to reduced movement. Over time, this also impacts the rest of your body! It is important to optimize full body functionality when treating pain.
5. From there, there may be emotional and mental stress also associated. Pain in the body is so complex, especially pelvic pain. Due to the nature of pelvic pain, it can be hard to talk about and there can be a lot of shame associated with it. Pelvic pain can also cause frustration because it is hard to see and describe. Overtime, this adds up and the additional fear and anxiety associated with the pain may actually make it worse!
Then, the cycle continues as it is perpetuated by these factors.
How to Fix Pelvic Pain?
If you have not already stumbled upon it, check out our blog titled “Pelvic Floor Therapist’s Guide: How to Treat Pelvic Pain”. This is a helpful resource for getting to know where to begin when it comes to pelvic pain. The TLDR or “Too Long Didn’t Read” version is that it all starts with finding a pelvic floor therapist that is equipped with the specialty skills to handle complex pain. At Bloom Pelvic Therapy, we are skilled in treating the most complex pelvic pain cases, working alongside your medical team to ensure you have the most superb care possible.
How Does Pelvic Therapy Help?
In an evaluation at Bloom Pelvic Therapy, you will spend at least 1 hour with your pelvic floor therapist to share your story and finally be heard. Clear answers start with having the opportunity to share details of your concern in a safe and comfortable setting where you are not rushed or dismissed. After discussing with your pelvic therapist and sharing additional medical history, your pelvic therapist may complete an internal muscle assessment of your pelvic floor, as well as assess whole body movement to better understand the cause of your concerns.
As the root cause of your symptoms are better understood and communicated with you, you will create a plan for your care with your pelvic floor therapist. This will guide your upcoming sessions and ensure the goals that are most important to you are of utmost priority and are met.
Follow up appointments will be based on your unique plan and may include hands-on manual techniques externally, such as myofascial release, or internally. Internal manual therapy techniques are provided either vaginally or rectally (depending upon which muscles are affected) often to decrease tension in pelvic floor muscles or fascial restriction. Outside of manual therapy, there are also movement-based strategies you will go through with your pelvic floor therapist. This may look like stretching, breathwork, and mindfulness. This could also look more like your workout or simulations of the way you do daily tasks. It all depends on you and which interventions your body needs.
Each session concludes with making sure you feel great, understanding where you are with your progress, and what you could be doing at home between the sessions. You will leave each visit with increased understanding and actionable items to progress you in reaching your goals.
We Are Here to Help You
Knowledge is power when it comes to better understanding your pain. Though this experience is difficult, we want to remind everyone that they are not alone. We are here to both listen and help you start breaking this cycle.
References:
Louw, A., Hilton, S., & Vandyken, C. (2014). Why pelvic pain hurts. International Spine and Pain Institute.
American Institutes for Research (2021). Moving from the cycle of pain to a cycle of Wellness.